Here are the guidelines for using insulin for diabetes

Guidelines for using insulin for diabetics
Insulin is a hormone that your body produces to help convert the food you eat into energy. People with diabetes might need insulin injections either because they don’t produce enough insulin in their bodies or they can’t properly use the insulin that they do produce or both.
Insulin injections have come a long way since they were first used to treat diabetes in the 1920s.There are not only different types of insulin to meet each user’s individual needs, but also different ways to inject insulin.
Also read: 3 Simple Steps To Prevent Gestational Diabetes
The insulin injection process itself has become easy and virtually painless. Insulin is like a key that opens up the locks on your body's cells so that glucose (blood sugar) can get inside and be used for energy. Insulin Helps Glucose Get Into Your Body's Cells. If the glucose can't get into your cells, it builds up in your blood stream. If left untreated, high blood glucose can cause long-term complications.
Additionally, when blood sugar reaches a certain level, the kidneys try to get rid of it through urine - which means that you'll need to urinate more often. Frequent urination can make you feel tired, thirsty, or hungry. You may also start losing weight. Your body also gets energy from a complex sugar called glycogen, which is stored in your liver and muscles. The liver converts glycogen to glucose and releases it into your bloodstream when you're under stress and/or when you're extremely hungry. When enough insulin is present, muscles can use their glycogen for energy, but cannot release it directly into the blood.
In type 2 diabetes, the liver releases too much glucose, especially at night (when the liver normally releases some glucose), resulting in high blood sugar levels in the morning. Insulin injections help bring down the amount of glucose released by the liver during the night, bringing morning blood sugars levels back to normal. Carbohydrates are broken down into glucose, which is the "fuel" that gives our bodies energy. Insulin's important job is to help glucose get into the body's cells.
Insulin Helps Build Muscle
When you've been sick or injured, or if you're recovering from surgery, insulin helps you heal by bringing amino acids (the building blocks of muscle protein) to your muscles. Amino acids repair muscular damage and help them regain their size and strength. If there isn't enough insulin in your body when your muscles have been injured, amino acids can't do their job, and your muscles can become very weak
Type of Insulin with time action
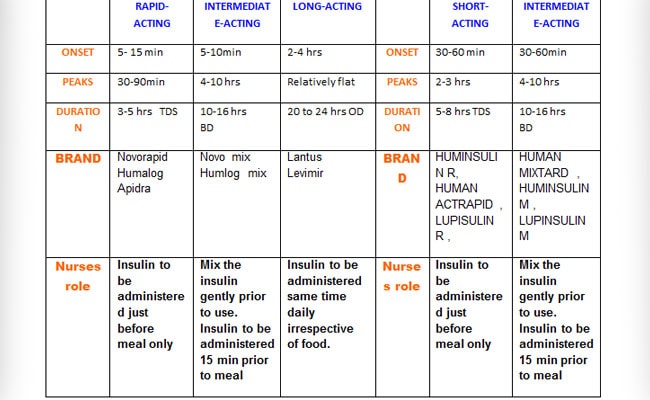
All about insulin usage
Photo Credit: Dr Sujeet Jha
1. Basal-Bolus Therapy
2. Premix insulin Therapy
Basal-Bolus Therapy
Combination 3 rapid or short acting and long acting Insulin
This type of insulin regime is referred to as a ‘BASAL BOLUS’ REGIME. The basal (background) insulin is given once a day and provides slowly absorbed background insulin over a 24 hour period. The bolus insulin (rapid t acting) is given three times a day before/with each meal and provides a quick insulin response to reduce blood sugars after a meal.
This regime offers the most flexibility as people can vary their doses for each meal, and will find that they don’t have to take extra snacks to maintain their blood sugars. They are often less likely to have problems with hypoglycemia or weight gain.
Background (Basal) ( LANTUS , LEVEMIR TRESIBA ) at bedtime and
Rapid/ short acting (bolus) (NOVORAPID , HUMALOG , APIDRA ) - injected at breakfast, lunch and evening meal
Premix insulin
Premix insulin ( HUMALOG MIX , NOVOMIX ,) has a faster onset of action than biphasic human insulin and should generally be given immediately before a meal. When necessary, Novo Mix 30 can be given soon after a meal
Premix insulin is biphasic insulin, which contains 30% soluble insulin aspart which has a rapid onset of action , thus allowing it to be given closer to a meal (within zero to 10 minutes of the meal) and the crystalline phase (70%) consists of protamine-crystallised insulin aspart, which has an activity profile that is similar to that of human NPH insulin act mainly upto 12 hrs but can last upto 24 hrs.
Site of injection
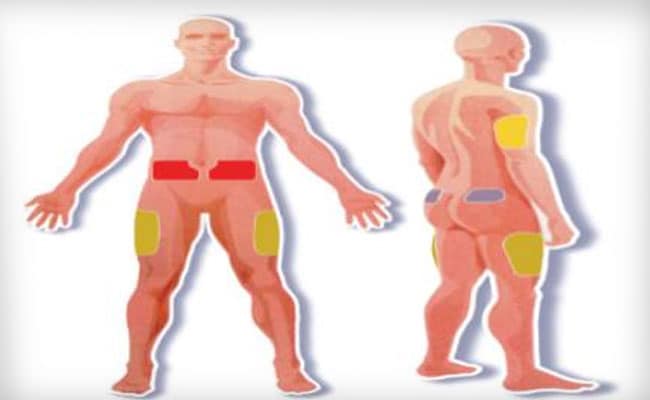
Photo credit: Dr Sujeet Jha
Injection technique
1. Pinch the site
2. Insert the needle at 90* angle
3. Deliver the injection
4. Release the pinch
5. Count 1 to 10
6. Remove the needle
7. Never massage the site
Also read: Can Diabetes Put You At A Risk Of Cancer?
Note
1. Always change the site of injection.
2. Change the needle of insulin pen after every single use.
3. Insulin must be stored in refrigerator (door).
4. Never shake the insulin vigorously.
5. Never use the insulin once frozen.
6. Never administer insulin from above the cloths.
7. For 100 I.U Insulin Vial use 100 I.U Insulin Syringe
Diabetes and sick day rule
• In case of diarrhoea, vomiting or any illness, contact your endocrinologist as the blood glucose level may rise when you are sick
• Check your sugar level every 4hrs and make proper adjustments in dose for sugar medication
• Take your diabetes medication regularly
• If you find your sugar level is over 300mg/dl, do check your urine for ketones.
• Avoid dehydration, drink plenty of liquids (calorie free)/ water. And if you unable to eat solid foods, include some liquids with carbohydrates.
Also read: Another Risk Factor For Diabetes In Children - Insufficient Sleep
How to store and handle insulin
Always read the instructions that come with your insulin. Bottles of insulin, either open or unopened, generally last for one month when stored at room temperature (59 to 86°F). A bottle is considered open if its seal has been punctured. If you remove the cap but don't puncture the seal, the bottle is still considered unopened.
If stored in a refrigerator, unopened bottles are good until the expiration date printed on the bottle. Opened bottles that are stored in a refrigerator should be used within one month of being opened. Many people store their unopened bottles in the refrigerator and keep open bottles at room temperature because they find it uncomfortable to inject cold insulin.
Don't use bottled insulin past the expiration date printed on the label. And no matter what the expiration date is, throw away a bottle one month after you open it. To help you keep track, write the date that you opened the bottle on the bottle's label.
With insulin pens and their cartridges, storage life ranges from seven days to one month. Check the chart below for shelf life details on popular brands.
Insulin cartridges
3ML
Humalog (28 days)
Novorapid R (30 days)
Novomix 70/30 (7 days)
3 mL
Humuinsulin R (28 days)
Huminsulin N (14 days)
Novomix 70/30 (10 days)
Novorapid (28 days)
Lantus (28 days)
Levemir (42 days)
Prefilled pens
Humalog (28 days)
Actrapid or Hunsulin R (28 days)
NPH (14 days)
Novomix 70/30 (10 days)
Troubleshooting
There are two ways to tell when insulin is no longer good: poor performance and unusual appearance.
If your blood sugar stays high even though you're following your treatment plan, your insulin may have lost its effectiveness. Poor performance could be due to two things:
1. Your insulin bottle has been open for more than 28 days.
2. You have a lot of punctures in the rubber stopper because you take very small doses of insulin and you're getting close to the end of the bottle.
If your insulin has an unusual appearance, it's probably no longer effective. Here are some warning signs:
- Your insulin is cloudy when it is supposed to be clear.
- Your insulin is supposed to be cloudy but it has clumps, even after rolling it between your palms.
- Your insulin looks stringy.
- Your insulin has changed in color.
If you think your insulin has gone bad, don't take any chances: throw the bottle away immediately and open a new one.
Also read: Immunotherapy For Treating Type 1 Diabetes
Smart Tips for Insulin Storage
- Protect your insulin (bottles, pens, and cartridges) from extremes of hot and cold.
- Keep insulin out of direct sunlight (for example, don't store it on a sunny window sill).
- Never store your insulin in the freezer - once insulin is frozen, it loses its potency.
- Don't store your insulin near radiators, heat vents, ovens, air conditioners, etc.
- Don't leave your insulin in a closed car during very warm or cold months.
- If you're going to be outdoors for a while in hot or cold weather, store your insulin in an insulated case.
Blood glucose checks can be frustrating. Sometimes I think I am doing everything right - I know my target, I know the carb count of any food I'm about to eat, I know my insulin-to-carb ratio, and I understand my insulin sensitivity.
But even if I pay close attention to these factors, my blood glucose results can be mysteriously higher or lower than I expected. What people may not know is that of the many things that can influence blood glucose, insulin absorption is one of the most important. Let's look at some common misconceptions:
MYTH: My blood glucose should not be affected by where I take my shot, or where I insert the catheter for my pump. After all, insulin going in is insulin going in!
FACT: Actually, the injection site you pick can affect how quickly the insulin is absorbed. For example, insulin is usually absorbed faster in the abdomen - sometimes almost twice as fast - than in other sites such as the thigh or arm.
MYTH: Insulin will always be absorbed faster if I inject in my abdomen.
FACT: Well, not exactly. There are additional things to consider,
If you take your shot or place your pump catheter in a spot on your abdomen where there is more fat underneath the skin, insulin may be absorbed more slowly. For example, the middle of the abdomen may be fattier than the side. Even though it might seem more comfortable to take insulin here, because there are fewer nerve endings, your insulin may not be absorbed as quickly as you want.
You should avoid using the same injection site continuously, because this can cause scar tissue to build up. Scarring at infusion sites is often seen in pump wearers, or those who have had surgery, but it is also seen in any people who use the same injection site constantly. Scars can cause a slowdown in absorption. That’s why site rotation is recommended, whether you use a syringe, pen, or pump.
When you exercise, blood flow to your legs increases, which speeds insulin absorption. If you inject insulin into the thigh and then exercise, the insulin will be absorbed faster than if it was injected in the abdomen.
MYTH: Temperature does not significantly affect insulin absorption.
FACT: Actually, heat can cause blood vessels to increase in size. So avoid taking a hot bath, shower or sauna after you take insulin. It could cause you to have a low blood sugar reaction.
MYTH: Injection site and temperature are the only things that affect insulin absorption.
FACT: That’s not quite true … there are rarely “absolute” rules with respect to diabetes,
• Exercising
• Injecting into a muscle (by using a needle that’s too long, or by not pinching up)
• Dose size
• Dose errors (take your time!)
MYTH: The type of food you eat does not affect insulin absorption.
FACT: True, but it can affect your blood sugar. Your body processes different foods at various rates. This can affect the relationship between your blood sugar and the insulin you take. For example, foods that are high in fat are typically absorbed slowly. Your insulin can “run out” before the food is absorbed entirely, causing a large swing in blood glucose. That’s another reason to go easy on foods like pizza and fries! Also, foods with a high glycemic index (such as rice) enter your system faster than foods with a low glycemic index, such as meat.
MYTH: As long as I use up my insulin within a month of receiving it, I don’t have to worry about how I store it.
FACT: It’s easy to forget, but insulin storage is critical to ensure its stability, which can affect absorption. Check the insulin package insert for storage guidelines. Vials that are currently in use can be kept at room temperature – avoid exposing them to extreme heat or cold. Keep all other unopened vials in the refrigerator. Never put your insulin in checked baggage when you fly: the luggage hold could get a lot colder than your fridge. Insulin that has been frozen and thawed should be thrown away, no exceptions, If you leave your opened insulin vials at room temperature, be sure the sun does not shine on them and heat up the contents while you’re out for the day. It’s a good idea to get into the habit of inspecting vials currently in use to ensure that the insulin has not crystallized. If the insulin that’s supposed to be clear has gone cloudy, or you can see what looks like salt inside the vial, do not use it! The insulin may be less effective, it might act unpredictably, or it might not work at all.
This may seem like a lot to keep track of, but remember: knowledge is power. The smarter you are about your diabetes, and insulin in particular, the better choices you can make to help you stay in good control. As always, be sure to check with your healthcare team before making any changes to your insulin injection routine.
DoctorNDTV is the one stop site for all your health needs providing the most credible health information, health news and tips with expert advice on healthy living, diet plans, informative videos etc. You can get the most relevant and accurate info you need about health problems like diabetes, cancer, pregnancy, HIV and AIDS, weight loss and many other lifestyle diseases. We have a panel of over 350 experts who help us develop content by giving their valuable inputs and bringing to us the latest in the world of healthcare.














